Menu
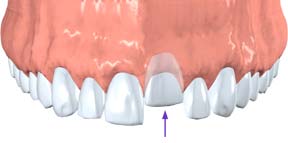 During an injury, a tooth may be pushed sideways, out of or into its socket. Your endodontist or general dentist will reposition and stabilize your tooth. Endodontic Therapy (root canal treatment) is usually needed for permanent teeth that have been dislodged and should be started a few days following the injury. Medication such as calcium hydroxide may be put inside the tooth as part of the Endodontic Therapy (root canal treatment). A permanent root canal filling will be placed at a later date.
During an injury, a tooth may be pushed sideways, out of or into its socket. Your endodontist or general dentist will reposition and stabilize your tooth. Endodontic Therapy (root canal treatment) is usually needed for permanent teeth that have been dislodged and should be started a few days following the injury. Medication such as calcium hydroxide may be put inside the tooth as part of the Endodontic Therapy (root canal treatment). A permanent root canal filling will be placed at a later date.
 Children between seven and 12 years old may not need Endodontic Therapy (root canal treatment) since their teeth are still developing. For those patients, an endodontist or dentist will monitor the healing carefully and intervene immediately if any unfavorable changes appear. Therefore, multiple follow-up appointments are likely to be needed. New research indicates that stem cells present in the pulps of young people can be stimulated to complete root growth and heal the pulp following injuries or infection.
Children between seven and 12 years old may not need Endodontic Therapy (root canal treatment) since their teeth are still developing. For those patients, an endodontist or dentist will monitor the healing carefully and intervene immediately if any unfavorable changes appear. Therefore, multiple follow-up appointments are likely to be needed. New research indicates that stem cells present in the pulps of young people can be stimulated to complete root growth and heal the pulp following injuries or infection.
If a tooth is completely knocked out of your mouth, time is of the essence. The tooth should be handled very gently, avoiding touching the root surface itself. If it is dirty, quickly and gently rinse it in water. Do not use soap or any other cleaning agent, and never scrape or brush the tooth. If possible, the tooth should be placed back into its socket as soon as possible. The less time the tooth is out of its socket, the better the chance for saving it. Call a dentist immediately!
 If you cannot put the tooth back in its socket, it needs to be kept moist in special solutions that are available at many local drugstores (such as Save-A-Tooth). If those solutions are unavailable, you should put the tooth in milk. Doing this will keep the root cells in your tooth moist and alive for a few hours. Another option is to simply put the tooth in your mouth between your gum and cheek. Do not place the tooth in regular tap water because the root surface cells do not tolerate it.
If you cannot put the tooth back in its socket, it needs to be kept moist in special solutions that are available at many local drugstores (such as Save-A-Tooth). If those solutions are unavailable, you should put the tooth in milk. Doing this will keep the root cells in your tooth moist and alive for a few hours. Another option is to simply put the tooth in your mouth between your gum and cheek. Do not place the tooth in regular tap water because the root surface cells do not tolerate it.
Once the tooth has been put back in its socket, your dentist will evaluate it and will check for any other dental and facial injuries. If the tooth has not been placed back into its socket, your dentist will clean it carefully and replace it. A stabilizing splint will be placed for a few weeks. Depending on the stage of root development, your dentist or endodontist may start Endodontic Therapy (root canal treatment) a week or two later. A medication may be placed inside the tooth followed by a permanent root canal filling at a later date.
The length of time the tooth was out of the mouth and the way the tooth was stored before reaching the dentist influence the chances of saving the tooth. Again, immediate treatment is essential. Taking all these factors into account, your dentist or endodontist may discuss other treatment options with you.
 Due to more sophisticated procedures, dentists are helping people keep their teeth longer. Because people are living longer and more stressful lives, they are exposing their teeth to many more years of crack-inducing habits, such as clenching, grinding, and chewing on hard objects. These habits make our teeth more susceptible to cracks.
Due to more sophisticated procedures, dentists are helping people keep their teeth longer. Because people are living longer and more stressful lives, they are exposing their teeth to many more years of crack-inducing habits, such as clenching, grinding, and chewing on hard objects. These habits make our teeth more susceptible to cracks.
Cracked teeth show a variety of symptoms, including erratic pain when chewing, possibly with release of biting pressure, or pain when your tooth is exposed to temperature extremes. In many cases, the pain may come and go, and your dentist may have difficulty locating which tooth is causing the discomfort.
To understand why a cracked tooth hurts, it helps to know something about the anatomy of the tooth. Inside the tooth, under the white enamel and a hard layer called the dentin, is the inner soft tissue called the pulp. The loose pulp is a connective tissue that contains cells, blood vessels and nerves.
When the outer hard tissues of the tooth are cracked, chewing can cause movement of the pieces, and the pulp can become irritated. When biting pressure is released, the crack can close quickly, resulting in a momentary, sharp pain. Irritation of the dental pulp can be repeated many times by chewing. Eventually, the pulp will become damaged to the point that it can no longer heal itself. The tooth will not only hurt when chewing but may also become sensitive to temperature extremes. In time, a cracked tooth may begin to hurt all by itself. Extensive cracks can lead to infection of the pulp tissue, which can spread to the bone and gum tissue surrounding the tooth.
There are many different types of cracked teeth. The treatment and outcome for your tooth depends on the type, location, and extent of the crack.
Craze lines are tiny cracks that affect only the outer enamel. These cracks are extremely common in adult teeth. Craze lines are very shallow, cause no pain, and are of no concern beyond appearances.
 Fractured Cusp
Fractured CuspWhen a cusp (the pointed part of the chewing surface) becomes weakened, a fracture sometimes results. The weakened cusp may break off by itself or may have to be removed by the dentist. When this happens, the pain will usually be relieved. A fractured cusp rarely damages the pulp, so Endodontic Therapy (root canal treatment) is seldom needed. Your tooth will usually be restored with a full crown by your dentist.
 Cracked Tooth
Cracked ToothThis crack extends from the chewing surface of the tooth vertically towards the root. A cracked tooth is not completely separated into two distinct segments. Because of the position of the crack, damage to the pulp is common. Endodontic Therapy (root canal treatment) is frequently needed to treat the injured pulp. Your dentist will then restore your tooth with a crown to hold the pieces together and protect the cracked tooth. At times, the crack may extend below the gingival tissue line, requiring extraction. A nontreatable tooth is  shown in the graphic above.
shown in the graphic above.
Early diagnosis is important. Even with high magnification and special lighting, it is sometimes difficult to determine the extent of a crack. A cracked tooth that is not treated will progressively worsen, eventually resulting in the loss of the tooth. Early diagnosis and treatment are essential in saving these teeth.
A split tooth is often the result of the long term progression of a cracked tooth. The split tooth is identified by a crack with distinct segments that can be separated. A split tooth cannot be saved intact. The position and extent of the crack, however, will determine whether any portion of the tooth can be saved. In rare instances, endodontic treatment and a crown or other restoration by your dentist may be used to save a portion of the tooth.
 Vertical Root Fracture
Vertical Root FractureVertical root fractures are cracks that begin in the root of the tooth and extend toward the chewing surface. They often show minimal signs and symptoms and may therefore go unnoticed for some time. Vertical root fractures are often discovered when the surrounding bone and gum become infected. Treatment may involve extraction of the tooth. However, endodontic surgery is sometimes appropriate if a portion of the tooth can be saved by removal of the fractured root.
Unlike a broken bone, the fracture in a cracked tooth will not heal. In spite of treatment, some cracks may continue to progress and separate, resulting in loss of the tooth. Placement of a crown on a cracked tooth provides maximum protection but does not guarantee success in all cases.
The treatment you receive for your cracked tooth is important because it will relieve pain and reduce the likelihood that the crack will worsen. Once treated, most cracked teeth continue to function and provide years of comfortable chewing. Talk to your endodontist about your particular diagnosis and treatment recommendations. S/he will advise you on how to keep your natural teeth and achieve optimum dental health.
Your teeth are held in place by roots that extend into your jawbone. Front teeth usually have one root. Other teeth, such as your premolars and molars, have two or more roots. The tip or end of each root is called the apex. Nerves and blood vessels enter the tooth through the apex. They travel through a canal inside the root, and into the pulp chamber. This chamber is inside the crown (the part of the tooth you can see in the mouth).
During Root canal therapy (Endodontic treatment), the canals are cleaned. Inflamed or infected tissue is removed. An apicoectomy may be needed when an infection develops or won’t go away after root canal treatment or retreatment.
Root canals systems are very complex, with many small branches off the main canal. Sometimes, even after Root canal therapy (Endodontic treatment), infected debris can remain in these branches. This can possibly prevent healing or cause re-infection later. In an apicoectomy, the root tip, or apex, is removed along with the infected tissue. A filling is then placed to seal the end of the root.
An apicoectomy is sometimes called endodontic microsurgery because it is often done using an operating microscope.
If a root canal procedure has been done in the past and it becomes infected again, it’s often because of a problem near the apex of the root. In many cases, a second Root canal therapy (Endodontic treatment) is considered before an apicoectomy. With advances in technology, endodontists often can detect other canals that were not adequately treated. In this case, they may be able to clear up the infection by doing a second root canal procedure. This will avoid the need for an apicoectomy.
Our endodontists can do an apicoectomy to fix the problem so the tooth doesn’t need to be extracted. An apicoectomy is done only after a tooth has had at least one root canal procedure and retreatment has not been successful or is not possible. For example, retreatment is often not a good option when a tooth has a crown or is part of a bridge. Retreatment of the root canal would require cutting through the crown or bridge. That might destroy or weaken the crown or bridge. An apicoectomy is often considered in a situation like this.
An apicoectomy is not the same as a root resection. In a root resection, an entire root is removed, rather than just the tip.
 Preparation
PreparationBefore the procedure, you will have a consultation with one of our dentists. We will also review your medical history. Depending on other existing medical conditions, we may consult with your physician before the procedure.
Before the surgery, you may be given an antimicrobial mouth rinse, a medicine to reduce inflammation, and/or antibiotics.
The endodontist will incise and lift the gum away from the tooth to gain access to the root. The infected tissue will be removed along with the last few millimeters of the root tip. The endodontist will use a dye to highlight cracks and breaks in the tooth. If the tooth has large cracks or breaks, it may have to be extracted. In this case, the apicoectomy will not continue.
To complete the apicoectomy, the endodontist will clean and seal the end of the tooth’s canal. The cleaning usually is done under a special microscope using ultrasonic instruments. The light and magnification allow the endodontist to see the area clearly. This increases the chance that the procedure will succeed. The endodontist then will take an X-ray of the area before stitching the tissue back in place.
Most apicoectomies take 30 to 60 minutes. The length will depend on the location of the tooth and the complexity of the root structure. Procedures on front teeth are generally the shortest. Those on lower molars generally take the longest.
We will send you home with written after-care instructions. Your endodontist will tell you which medicines to take and what you can eat or drink. You should apply ice to the area for 10 to 12 hours after the surgery, and rest during that time.
The area may bruise and swell. It may be more swollen the second day after the procedure than the first day. Any pain usually can be controlled with over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil, Motrin and others). In some cases, you may be given a prescription pain medicine.
To allow for healing, you should avoid brushing the area or rinsing vigorously until your follow-up appointment. Also, don’t smoke or eat crunchy or hard foods. Do not lift your lip to examine the area. This can loosen the stitches and disrupt formation of the blood clot that is needed for healing.
You may have some numbness in the area for days or weeks after the surgery. Tell your endodontist about any numbness. The numbness usually goes away with time.
Your stitches will be removed approximately 7 days after the procedure. All soreness and swelling are usually gone within 14 days.
Even though an apicoectomy is considered surgery, many people say that recovering from it is easier than recovering from the original Root canal therapy (Endodontic treatment).
The endodontist will review the risks of the procedure at the consultation visit. The main risk is that the surgery may not work and the tooth may need to be extracted.
Depending on where the tooth is located, there may be other risks. If the tooth is in the back of your upper jaw, the infection can involve your sinuses. Your endodontist may suggest antibiotics and decongestants.
The roots of the back teeth in the lower jaw are close to some major nerves. Surgery on one of these teeth carries a slight risk of nerve damage. The chances of anything happening are extremely small; however, your endodontist will use your X-rays to see how close the roots are to the nerves.
An apicoectomy is usually a permanent solution. It should last for the life of the tooth.
Root canal retreatment is a procedure used to clean the canals of a tooth that have already been subject to a root canal. Although most root canals are successful the first time, there are many reasons why a retreatment may be necessary. For example, some patients may have hidden canals that were not identified in the initial procedures, whereas others may experience a new infection caused by a loose crown or damaged filling. In some cases, these complications can occur immediately following a root canal when pain continues to persist and the tooth fails to heal. For other patients, complications can arise many years after an initial root canal. The goal of re-treatment is always the same as the initial root canal: Eliminate all bacteria from the inside of the tooth and seal it so that it is permanently protected from future infections.
Did you know…
that a retreated root canal can allow a natural tooth to last many years or even a lifetime? In fact, the National Institutes of Health confirm that successful treatment is a realistic goal of root canal retreatment. As with any dental procedure, there is no guarantee that retreatment will be a success for every patient. However, the majority of root canal retreatment patients – approximately 70 percent – experience positive outcomes.
If your root canal treatment was unsuccessful or a new infection has occurred in a previously treated tooth, retreatment offers a chance to save your tooth without having it extracted. If many years have passed since your initial root canal, innovative new methods may be available to your endodontist that were not an option during your first treatment. Of course, there is no way to know whether retreatment is right for you without first consulting with your endodontist.
If you determine that retreatment is right for you, your tooth will be reopened so that the filling may be removed from your tooth. Special instrumentation will be used to identify hidden canals or areas of the tooth that could be harboring an infection. These areas will be cleaned out and refilled. You’ll then return to your dentist for a crown or other type of restoration.
As with your first root canal, your retreatment will require you to avoid chewing or biting with your treated tooth until you can return to your dentist for a restoration. You may also experience some discomfort following your treatment. These usually subside within a few days, but contact your endodontist if pain persists or worsens.
Root canal treatment is an endodontic procedure used to clear infected pulp away from the pulp chambers and canals of a diseased tooth. Infections occur when bacteria are allowed to enter the pulp – often due to untreated decay or a crack in the tooth. During a root canal, the tooth is opened and the pulp removed. Biocompatible cement is used to fill the tooth before it is restored with a crown or other restoration.
Did you know…
that while most infected teeth are easily identified by the symptoms they cause, some produce no discomfort at all? It is important to visit your dentist regularly for routine exams that may reveal diseased teeth that would otherwise go unnoticed. Failure to treat an infected tooth could result in the death of the tooth and total loss. Worse, the infection can spread to other areas of the body, causing potentially life-threatening conditions.
You may need a root canal if tooth decay or a broken tooth has allowed the pulp to become infected and inflamed. Signs and symptoms to watch out for include temperature sensitivity, swelling, drainage, odor, pain, and discoloration of the tooth. It is important to treat infections quickly, as delaying treatment can result in severe tooth pain and abscess.
Your endodontist will numb your tooth with a local anesthetic and administer analgesia if needed. Once the tooth is numb, an opening will be made in the top of your tooth to access the canals. Your endodontist will use tiny instruments to remove pulp from your tooth and prepare it to be filled. You will return at a later date to have your root canal capped with a crown or other type of restoration that will give it the appearance and function of a natural tooth.
You will be allowed to drive yourself home from your root canal visit and may even wish to return to work the same day. However, it is normal for your tooth to be sensitive in the days following your procedure. You’ll need to avoid biting anything with your filled tooth, as this can cause it to break or fracture. So long as the tooth heals normally and you experience no complications, you can return to your endodontist within a month to have a crown or other restoration placed on the tooth.